Anatomy of Kidney
The two kidneys lie against the back abdominal wall, lateral to the spine, in the lumbar region.
Left kidney is located caudally and right kidney cranially to head.
Role of Kidney
Bone health
Blood pressure
Acid – base balance
Erythropoietin
Water regulator
Renal dysfunctions
Renal insufficiency: >70% loss of functional mass= Loss of concentrating ability leading to dilute urine.
Risk factor
Age:Highest risk factor at age of >8 years, sometimes 4-8 years and lowest risk factor at age of <4 year.
Gender: It is not specific but higher in female than male
Breed: Labrador > German shepherd > Pomerian
Disease: Systemic Infectious disease
Cardiovascular disorder and obstructive causes
Food: High phosphorus and high protein rich diet and
Managmental: Obesity, trauma and expose to toxin
Etiological Agent
Infectious cause:
A. Viral infection : it is not specific right now
B. Bacterial infection : Leptospirosis , Pyelonephritis
C. Haemoprotozoan infection : Borelliosis,
Systemic causes:
A. Sepsis
B. Urolithiasis
C. Nephroliths
D. Hyper calcemia
Drugs:
A. Aminoglycosides
B. NSAIDs
C. ACE blockers
D. Radiographic agent
Miscellaneous:
A. Ischemia
B. Shock
C. Infraction
D. Pancreatitis
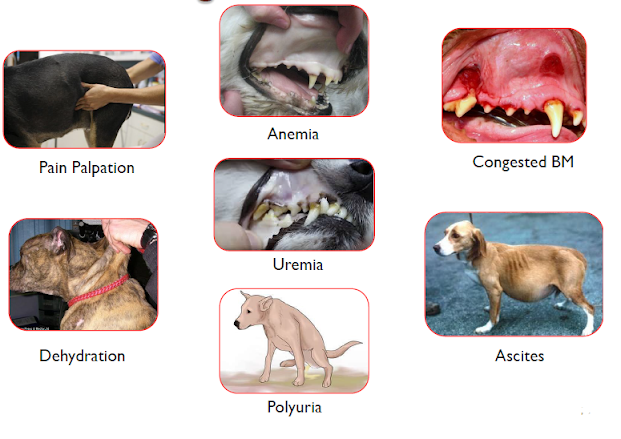
Clinical Sign:
Persistent Vomiting.
Polyuria-polydipsia followed by oliguria.
Various degree of dehydration.
Anaemia
Lethargy, halitosis and paresis
Haemorrhages on buccual mucosa and melena
Oedema of hind limbs
Ascites
Diagnosis
1. History and Clinical Signs
2. Physical examination
3. Urine analysis
4. Haematology
5. Serum Biochemistry
6. Biomarkers
7. Ultrasonography and Radiography
8. Biopsy
Urine Analysis
Non-invasive method of assessing the function of kidney.
Fresh urine should be collected for analysis either through direct voiding (mid–stripe) or catheter.
Physical Examination of Urine
|
Parameters |
Normal |
Alterations |
|
Color |
Yellow due to Urochrom |
Deep yellow–Dehydration Colorless –Diluted / Isothuria |
|
Volume |
20-25 ml/kgB.wt./day |
Polyuria-Earlystage Oligouria-Later stage Anuria-End Stage |
|
Specific Gravity |
1.015-1.030 |
Increased -Early stage (1.050-1.076:5% dehydration) Decreasein -Later stage |
Chemical Examination of Urine
|
Parameters |
Normal |
Alteration |
|
pH |
5.0 –7.5 |
•Decrease–Acidosis, Protein rich diet •Increase–UTI, diuretics, alkalosis
|
|
Glucose |
Not present |
>180mg/dL–Diabetes Mellitus |
|
Blood |
Not present |
Haemoglobinuria(Haemolysis, Autoimmune reaction), Haematuria(Trauma) |
|
Protein |
Trace <50mg/dL |
If higher (++) suggestive of •Renal damage, glomerulonephritis, cystitis and urethritis. •Non-renal causes: PLE, hemo and myoglobinuria, heavy exercise and diet
|
Hyaline casts -Mild stage of renal impairment.
Granular casts– it is the hallmark of acute kidney injury due to ischemia, protein induced nephropathy viz. haemoglobin and myoglobin, administration of nephron toxic drugs etc.
Epithelial cell casts -Acute nephritis and cystitis.
Fatty casts –Damage in renal tubules seen in DM.
Erythrocytic casts –Haemorrhage in the kidney /RT.
Leukocytic casts -Inflammation and Sepsis.
Haematology
Normocytic normochromic and regenerative anaemia is commonly observed in acute form while Non-regenerative anaemia is one of the common findings in dogs with chronic kidney dysfunctions.
PCV is usually increased.
Neutrophilia and leucocytosis suggest sepsis.
In renal disorders due to hemoprotozoan infections, thrombocytopenia is a common finding.
Serum Biochemistry
In General screening following tests are to be done for assessing degree of renal damage.
1. Blood Urea Nitrogen / Urea
2. Creatinine
3. Sodium and Potassium
4. Phosphorous and Calcium
5. Total protein
Urea and BUN(Normal:10-30mg/dL):
Urea is end product from ammonia derived from protein catabolism within the liver and filtered at glomerulus.
Urea is about 2.14 times than BUN Thus, BUN 10mg/dL is equivalent to urea 21.4mg/dL.
It is an insensitive indicator of reduced GFR.
When GFR reduced by around 50% ,BUN gets elevated above the upper limit.
Creatinine (Normal:0.5-1.5mg/dL):
It is produced from dehydration of creatine and dephosphorylation of phosphocreatinein muscle.
It specific indicator of renal involvement but less reliable because its elevation seen when 75%loss of functional nephrons.
Creatinine has an exponential relationship with GFR.
Hence, normal creatinine values can camouflage the renal involvement in routine clinical practice.
Hyperphosphetemia
Whenever decrease the GFR rate and increase Phosphorus concentration in kidney so there is poor calcium absorption so there will be also decrease calcitrol and increase parathyroid hormone which lead demineralization of bone and increase the phosphorus in tissue.
Hypokalaemia
The ability to maintain potassium extraction at near normal level in generally maintained by aldosterone secretion and distal flow rate
Common source of low aldosterone level are Diabetes mellitus, use of ACE inhibitors, NSAIDs or beta blockers
Hyperkalaemia is consistent finding in advanced stages of kidney disease.
Symmetric dimethylated arginine (SDMA)
It is a sensitive indicator of kidney function that detect as little as 25% loss of function
It is not influenced by muscle mass and an early indicator of progressive kidney function loss as well as concurrent disease that may have a secondary impact of kidney function
Biomarkers of kidney dysfunction
Urinary markers of glomerular dysfunction
Albumin microalbuminuria
C reactive protein acute phase proteins with and increased serum concentration in inflammatory disease
Due to its size 115 k Dalton CRP is not able to pass through the impact glomerular barrier the presence of CRP in urine is the result of glomerular dysfunction
Ultrasonography
Ultrasound is the ideal imaging test of evaluating Kidney Disease because it provides information about the position site safe internal architecture of Kidneys without harming the patient
Disease of kidney treatment by ultrasonography can be divided into
1. Diffuse: nephritis ESKD
2. Regional: hydronephrosis PN and nephroliths
3. focal for multifocal like cyst or Polycystic in renal disease.
Measurement of renal size by
i. Renal : centimetre
ii. Kidney and Aorta (K/Ao) = 5.5 to 9.1 centimetre
Radiography
It is useful to determine chronic kidney is function when mineralization from bone mineralization to other tissue developed.
Renal biopsy
Renal biopsy is considered for patient with…
Persistent substantial proteinuria
Unresponsive to antiproteinuric therapy
Suspecting renal mass and CKD in young dogs
Glucose platelet buccal mucosal bleeding time and blood pressure should be with reference range
Acute kidney dysfunction (AKD)
The functional or structural abnormalities for markers of kidney damage including abnormalities and blood urine or tissue test for imaging study present for less than 3 months
|
AKI Grade |
Serum Creatinine (mg/dl) |
Clinical description |
|
|
Grade 1 |
<1.6 |
Non azotemic AKI •Clinically oliguria/anuria, •Nausea/vomition •Elevation/ detection of biomarker
|
|
|
Grade 2 |
1.7-2.5 |
Mild AKI •Increase in S.Creatinine≥ 0.3 mg/dl within 48 h and VR: < 1ml/kg/h over 6 h
|
|
|
Grade 3 |
2.6-5.0 |
Moderate to Severe AKI •Severities of clinical signs due
|
|
|
Grade 4 |
5.1-10.0 |
||
|
|
|||
Chronic kidney dysfunction
Structural and functional impairment of one or both Kidneys that has been present for more than approximately 3 month
Security is considered as disease of an older animals although it covers at all ages
|
Stage |
Blood Creatinine (mg/dl ) |
Serum SDMA (μg/dl) |
Comments |
|
1 |
1.5 |
14-18 |
Protinuria, Structural and function changes |
|
2 |
1.4 –2.8 |
18 -35 |
Mild systemic signs |
|
3 |
2.9 –5.0 |
36 -54 |
Moderate systemic sign |
|
4 |
>5.0 |
>54 |
Marked systemic and Uremic sign |
Differentiating points of AKI to CKI
|
PARAMETERS |
ACUTE |
CHRONIC |
|
Clinical signs |
Anorexia, lethargy and voimition |
Azotaemia more severe than clinical signs |
|
Water Intake/ Urine ,Body Cond. |
Reduced, Good |
PU/PD, weight loss |
|
Kidney size/ shape |
Normal/large with Pain |
Small and irregular architecture and no pain |
|
Haematology |
Non anaemic, PCV increased |
Non-regenerativeanemia |
|
K
P |
Normal to high
High |
Mild hyperkalemia
High |
|
Urine SG |
Pre Renal: > 1.030 Renal : 1.008 -< 1.030 |
1.008 -1.015 |
Principle of treatment
NEPHRONS
N management of Nutrition
E balance electrolytes
P regulate blood pressure and proteinuria phosphorus
H management of hydration
R management of retention of substance
O other renal insult avoid
N management of neuroendocrine function
S serial monitoring of patient
Management of dehydration
|
|
|||||
|
Degree of Dehydration (%) |
Eye ball position |
Skin tenting (sec.) |
HCT (%) |
Mucous Membrane of eye |
Capillary Refill Time (Sec) |
|
Normal |
Normal |
<1 |
40 |
Moist |
< 2 |
|
1-5 |
Normal |
1-4 |
40-45 |
Moist |
2 |
|
6-8 |
Slightly sunken |
5-10 |
50 |
Tacky |
2-3 |
|
9-10 |
Gap between eyeball and surrounding tissue |
11-15 |
55 |
Tacky to dry |
4 |
|
11-12 |
Large gap and very sunken |
16-45 |
60 |
Dry |
>4 |
Place IV catheter and urinary catheter
Fluid replace = percentage of dehydration × body weight in kg within 24 hours
5% dehydration on always present when kidney insult is established so it is replaced it within 2 to 4 hours
Maintenance fluid is to be given at 44 to 66 ml/kg/day
Choice of fluid will be RL solution, if not hyperkalemia. Otherwise 0.9 percentage sodium chloride
Give 10 ml/kg IV crystalloid, if no output of urine go for diuresis
Management
of Oliguria or Anuria
When fluid therapy initiated urinary flow should be rapidly increased to
>2 ml/kg body/hour
Oliguria: <0.5 to 1 ml/kg/hour
in spite of fluid therapy
Furosemide: Loop diuretic
and first choice
It will increase urinary flow without increasing GFR
It has been renal vasodilatory effect
It inhibit Na, Cl and K pump in luminal
cell of loop of henle
Dose: 2 ml/kg intravenously urine output is 30 to 60 min. If escalate
dose at 4-6 ml/kg body weight after 1 hour
CRI : 0.66 mg/kg/hr has been effective in dog
20%
mannitol osmotic diuresis second choice
It helps in extracellular volume expansion and inhibit renal sodium
absorption by acting as an antagonist
Increase renal blood flow GFR scavenging free radicals and solute
excretion
Dose 0.5 to 1 gram/kg body weight within 20 min. Urine flow increase
within our and repeat every 6 hours
CRI: 1 ml/kg/min intravenously
Avoid using oliguric patient with volume overloaded or 20% dextrose
22-66 ml/kg/day (2-10 ml/min)
Balance
of electrolyte
Metabolic acidosis is commonly occur in acute kidney and chronic kidney
infection
Alkalizing therapy should not be recommended unless blood pH is less
than 7.2 or serum bicarbonate level is less than 40 mEq/litre after correcting
fluid deficit
Give 1/4 to 1/2 dose directly by slow IV and remaining in IV fluid over
for 4 - 6 hour
Hyperkalemia
Renal excretion in the major mechanism of removal of K from body
It is life threatening not control
Insulin 0.5 unit/kg body weight IV followed by dextrose 2 gram (40ml
5D)/unit of insulin. Or 10% calcium gloconate at 0.5-1 ml/kg Slow IV will
restore cardiac abnormality within a minute
Management
of neuroendocrine function
Renal secondary hyperthyroidism occur commonly with CKD because of
phosphorus retention and decrease calcitriol
Calcitriol stimulant gastrointestinal absorption of calcium and
phosphorus inhibit parathyroid hormone production
Calcitriol 2 - 3 ml/kg/ day oral
after dissolution of hypercalcemia and hyperphosphatemia
Hypoproliferative
anaemia Hallmark of kidney dysfunction
It has been shown that patient with chronic kidney disease have
increased survival If the haematocrit it is about 35%.
Human Recombinant erythropoietin can be given at off 100 IU/kg body
weight SC trice in week
Darbepoetin, long acting erythropoietin also be used at 1mcg/kg body
weight SC once in a week
Blood
pressure
|
Risk assessment |
Systolic BP (mmHg) |
DiastolicBP (mmHg) |
Breed specific |
|
Minimal risk Normotension(N) |
<150 |
< 95 |
<10mmHg |
|
Low risk Borderline hypertension (BP) |
150-159 |
95-99 |
10-20mmHg |
|
Moderate risk Hypertension (H) |
160-179 |
100–199 |
20-40mmHg |
|
High risk Severe Hypertension( SH) |
>180 |
>120 |
>40mmHg |
|
Risk not determined |
No Blood Pressure not
measured |
||
Drugs
for Gastro-intestinopathy
For the control of Vomition:
1. Odansetron: 0.5 mg/kg b.wt. IV at every 6
hrs.
2. Metaclopromide: 0.2 mg/kg b.wt.IVat every
8 hrs.
3. Maropitant: 1mg/kg b.wt. SC SID < 5
days.
For the control of Gastric Ulcer:
1. Ome/ Penta-prazole(PPI) : 1mg/kg b.wt.
IV/PO SID.
2.
Sucralfate: 0.5 –1gm/kg b.wt. POTID
Nutritional
management
Protein restriction: BUN>80mg/dl, high P & Creatinine
2.5mg/dl.
Renal diet is required generally with CKD stage II–IV where
proteinuria is an evident.
Diet should have sufficient calories (70kcal/kg/day) to
stop protein catabolism.
No sodium restriction required.
Supplementation of Omega-3PUFAs (notO-6) have shown reno-protective
anti-inflammatory properties.
Commercial available renal wet diet is preferable.
Renal Replacement Therapy(RRT)
Indications:
·
When dog
failed to respond medical management.
·
Severe
hyperkalamia(>8 mEq/L), hyperphosphetemia(>10 mg/dL).
·
Persistent
uraemia signs.
·
Patient
with AKD has more appropriate than CKD.
RRT
can only extend longevity for few months and provides wellbeing of kidney
patients at high cost.
Peritoneal dialysis: removes uremic toxins by diffusion from the peritoneal
membrane.
Extracorporeal Renal Replacement Therapy(ERRT) removes uremic toxins by diffusion
and/ conventions from blood; can be performed by Intermittent Haemodialysis(IHD)
and Continuous Renal Replacement Therapy(CRRT) units.
Prognosis of kidney
dysfunction
Despite
all the advances, about 60% of dogs with this disease either die or are humanely
euthanized because of failure to respond to supportive care.
For
dogs with severe ARF treated with haemodialysis survival was nearly 80% for dogs
with infectious causes, 40% for dogs with non-infectious and non-toxic etiologies.
Decreased
urine production and hyperkalaemia are poor prognostic factors in dog kidney dysfunction.
Mean survival time for CKD patients is 226 days based of
IRIS stages.
References:
(IRIS, 2019)
Special
thanks to Dr.Sudhir A. Maheta , assistant professor, Department of veterinary
medicine, NAU, Gujarat.






💯🙌
ReplyDeleteGood and very important information
ReplyDeletePost a Comment