v EIA is inflammation and proliferation of the monocyte-macrophage and lymphoid systems which cause hypertrophy and hyperplasia particularly in the spleen and lymph nodes so resulting in splenitis and lymphadenitis.
v EIA is a retroviral disease of equids that may be characterized by acute and/or chronic recurring clinical signs including fever, anemia, edema and cachexia in some animals.
Synonyms
v Swamp Fever (it is contagious viral disease of horses that causes anaemia and emaciation and usually fatal.)
v Coggins Disease (Diagnosis by Coggins test)
v Mountain Fever(Tick)
v Slow Fever
v Equine Malarial Fever
v Vallee's disease
Etiology
v Equine infectious anemia virus
vGenus: Lentivirus
vSubfamily Orthoretrovirinae
vFamily: Retroviridae
vOnce infected become lifelong carrier.
Transmission
v Only Mechanical transmission (Not Biological)
v Mouthparts of biting insect
Horse flies, stable flies, deer fly
Bites painful→ Horses react → Fly feeding interrupted →Fly resumes feeding on same animal or nearby host → Infectious blood transferred to new host
v Fomites contaminated with blood Needles , Surgical instruments, Floats
v Route of minor importance Saliva, In utero, Via milk, Venereal , Aerosol
Pathogenesis
→ EIA is a blood borne infection. virus enter through penetrating wounds of the blood vascular system in the skin or either from fly (Horse flies, stable flies, deer flies) or mosquito bites or from contaminated needles.
→ Once virus in the bloodstream à free virus infects monocytes which are nonpermissive cells but they are not differentiated macrophages so virus cannot fully replicate
→ Thus monocytes spread virus in the circulatory system via leukocyte to all organs like spleen and Lymphnode and other systems
→ when Infected monocytes are migrate by blood vessel walls and enter ECM of tissues, where they differentiate into tissue macrophages these are permissive cells and resulting in splenitis and lymphadenitis
→ Infected macrophages produce proinflammatory chemokines and cytokines that recruit additional monocytes and lymphocytes into organs like spleen, lymphnode so seen splenomegaly and lymphadenomegaly.
How to produce anemia ?
→ Circulating viral antigen adsorbed to erythrocyte (RBCs)
→ RBCs: Antibody and C3 bind to the virus → extravascular hemolysis in this macrophage recognition of complement or haptens in spleen and other organs → lysis of cells → Anemia
→ Intravascular hemolysis in this Ab bind to viral Ag on RBC surface → activates complement cascade lysis of cells → Anemia
→ Circulating viral antigen adsorbed to platelets membranes also so Immune-mediated thrombocytopenia à platelets destroyed by similar mechanism or are activated and then bound by fibrinogen and phagocytosed
Clinical Sign
Two form: Acute and Chronic
Acute
→High
fever (up to 108oF)
→Depression,
anorexia, weakness, ataxia, weight loss
→Dependent
edema
→Petechial
(ventral tongue, ocular and vulvar mucosa) due to thrombocytopenia
→Anemia
→Icterus
(pre-hepatic)
Chronic
→The disease is caused by antigenic variation in antigenic drift/shift of
surface glycoproteins of the virus.
→Recurring
1-2 week cycles of fever
→Emaciation,
weakness
→Ventral
edema
→Anemia
and thrombocytopenia
→Lasts
8 to 12 months with decreasing frequency and severity of disease until
asymptomatic infection
→Asymptomatic
carriers may suffer relapse
Macroscopic Pathology
→Spleen
and lymph node
→Enlarged
spleen and lymph node
→Abundant
lymphoid follicles that bulge from the cut surface
→Capsular
hemorrhages
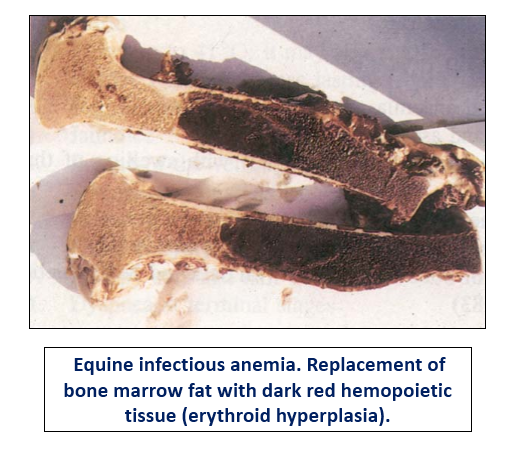
→Bone
marrow: The increase of reddening (hyperplasia of the hematopoietic marrow)
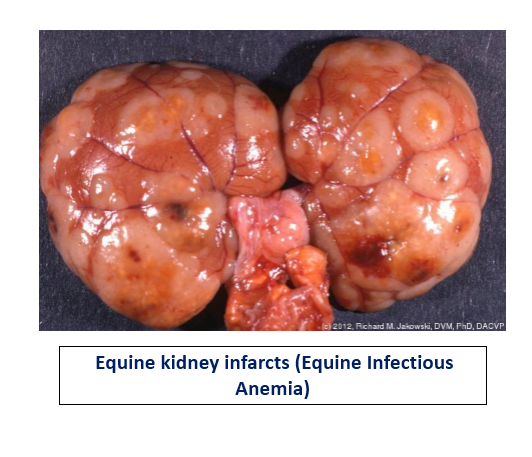
→Icterus,
widespread hemorrhagic foci, subcutaneous edema, pallor, and renal petechiae
→Liver: Enlarged, dark, and turgid with capsular hemorrhage
Microscopic Pathology
Acute:
→Prominent
lymphoid hyperplasia
→Hemosiderosis
in major organs
→Ischemic
necrosis of the heart, liver, and kidneys
→Bone marrow: Hypercellular with erythroid hyperplasia
Chronic:
→Monocyte/macrophage
hyperplasia with hemosiderosis
→Lymphoid
involution and atrophy
→Liver:
Atrophy, Kupffer cell hyperplasia, hemosiderosis
→Spleen:
Large follicles but hypocellular -"bull's eye”
→Bone
marrow: Hypercellular with erythroid hyperplasia
→CNS:
Granulomatous ependymitis and choroid plexitis
→Base on Clinical signs
→Laboratory tests
→Coggins
test: Agar gel immunodiffusion test
→Enzyme-linked immunosorbent assay (ELISA)
→Reverse-transcriptase polymerase chain reaction
→Serological tests
→ Hematological studies effect on EIA like..
→Normocytic Normochromic anemia
→Leukopenia, fall of P.C.V
→ Neutropenia, Thrombocytopenia
→ Elevated heinz body and Icterus index
[Varshney et al., 1994]
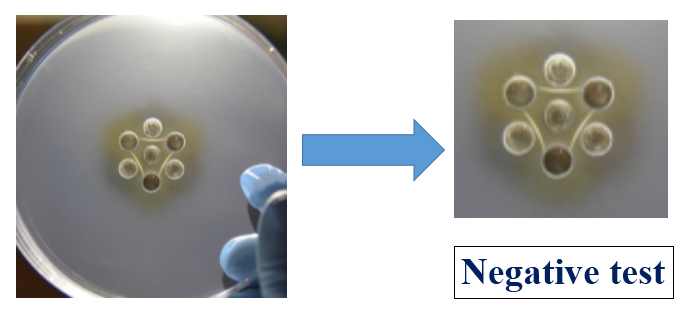
AGID -
Principle :
→The test is an Agar Gel Immuno-Diffusion (AGID) assay designed to detect the
presence of antibodies against virus in horse serum. The test uses a recombinant
protein consisting of the virus p26 core protein to detect the specific antibodies to
virus.
→Samples are added to 1% Noble Agar in a petri dish cut with a seven well template where EIAV Recombinant p26 Antigen is in the centre well and viruscPositive Control Reference Serum is added to every second well for a total of three virus Positive Control Serum wells for each seven well template.
→The remaining three
wells contain test samples.
→Samples positive for EIA virus specific antibodies react with the recombinant antigen to form an antibody antigen complex which is visualized as a precipitin line between the test well and the antigen well.
→Weaker samples may not form a complete precipitin line but instead change the migration pattern inward towards the sample well.
→Samples negative for EIA virus specific antibodies will not form a precipitin line with
the p26 antigen, nor will they cause a deviation of the EIA virus Positive
Reference Control Serum lines.
Process to prepare Gel.
1.Take a 9 grams of Boric Acid and dissolved in 1 liter distilled water.
2. Then 2 grams of Sodium Hydroxide is added to the borate buffer and allowed to mix until in solution. Alternatively a 50 x stock of sodium hydroxide may be used. The final concentration of the solution is 0.146 M Boric Acid, 0.05 M NaOH. The pH of the solution is measured. Acceptable range is pH 8.6 ± 0.2.
3. 10 grams of Noble Agar (1% w/v) is added to the solution and is mixed for a few minutes until it is in a homogenous suspension.
4. The suspension is then heated by microwave or hot plate until the agar is in solution.
5. The solution is allowed to cool for a few minutes and 15 mL is added to 100 mm diameter plastic petri dishes.
6. The agar is allowed to cool until it becomes firm, the lids are placed on the plates and they are then stored inverted at 2-8 °C, for up to 7 days, until use.
Cutting the Agar Gel:
A 7 in which one center well with six surrounding wells.
Procedure :
1. Add 50 µL of Antigen (Ag) to center well of the seven well pattern so that the solution is level with the top of the well.
2. Add 50 µL of Positive Control Reference Serum to every other well on the outside of the antigen well so that the solution is level with the top of the well.
3. Add 50 µL of sample to the remaining three wells in the pattern so that the solution is level with the top of the well.
a. A total of 3 samples may be tested per well pattern. If less than 3 samples are to be tested, fill remaining sample wells with a blank, such as Phosphate Buffered Saline (PBS).
4. Then incubate at room temperature (15-25 °C) in a closed humid chamber.
5. Read plate and record results at 24 hours.
6. If the reaction is complete after 24 hours, results may be reported. Weak positive samples may require up to 48 hours before the reaction is complete
Result






Thanks for support Dr
ReplyDeleteThanks Dr
ReplyDeleteWelcome Dr
DeleteThank You Dr
ReplyDeleteBest ever 👍🏻👍🏻
ReplyDeletePost a Comment