Introduction
- Jaundice is French word means yellow
- Icterus is Greek word means jaundice/yellow jaundice.
- Jaundice is sign, it is not a disease.
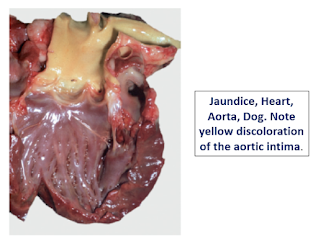
- Definition: It is the yellowish discoloration of the tissues, particularly those with high elastic tissue content, including the sclera and aorta, due to an increase in bilirubin termed hyperbilirubinemia.
Or
- A yellow discoloration of tissue that is especially evident in tissue rich in elastin, such as the aorta and sclera, due to increased concentration of conjugated or unconjugated bilirubin in blood.
- Normal Value: 0.5 -1.0 mg/ dL
- Discoloration occurs only when bilirubin levels
rise above 2.0 mg/dL. So the animal can be hyperbilirubinemic but not icteric.
Here, what is
jaundice and icterus / when we called that is jaundice or icterus?
- When an excessive accumulation of a yellow pigment into blood and tissues. This is known as an icterus.
- But when icterus has present for any length of time and discolor many tissues of body and that is become visible as jaundice on most body surfaces areas and the skin.
- In case of horses bilirubin have a wider reference range and may not be hyperbilirubinemic at this concentration. So maximum accumulation of bilirubin in tissues of horse takes approximately 2 days, and that’s why horse with acute hepatic failure or obstruction may have seen icterus.
- Unconjugated Bilirubin:in this Bilirubin is bound to a certain protein (albumin) in the blood is called unconjugated or indirect
- Conjugated Bilirubin: In the liver, bilirubin is conjugated with glucuronic acid by the enzyme glucuronyltransferase ans it is water soluble.
Mechanism how to develop Jaundice/icterus
- Overproduction of bilirubin due to increase hemolysis
- Reduced liver uptake due to lake of enzyme
- Impaired conjugation
- Impaired intrahepatic secretion of bilirubin due to
Hepatic
damage,
Intrahepatic
cholestasis and
Biliary
obstruction
- Impaired extrahepatic secretion of bilirubin due to bile duct obstruction.
Classification
of Jaundice
Haemolytic or prehepatic jaundice
- 80% or more of the serum bilirubin is unconjugated (unconjugated hyperbilirubinaemia)
- Overproduction of bilirubin
- Reduced liver uptake:
•
Certain drugs such as
rifampin, an antitubercular drug
- Impaired conjugation:
• Activity of glucoronosyl
transferase is low at birth – neonatal Jaundice
• Hereditary, or acquired
deficiency
Etiology
- Bacteria : Leptospirosis, Clostridium haemolyticum,
- Virus : Equine infectious anaemia (EIA)
- Protozoa : Babesiosis, Trypanosomosis Anaplasmosis, Haemobartonellosis,
- Nutritional : Phosphorus deficiency - Post parturient haemoglobinuria(PPH)
- Phytotoxins : Saponin, Resin.
- Animal toxin : Snake venom
- Chemicals : Copper and selenium toxicity in sheep
- Icterus neonatarum, incompatible blood supply
- Haemolytic anaemia
- Zn toxicity or onion toxicity
In to Blood Extravascular
or intravascular haemolysis
⇓
Unconjugated bilirubin in Blood
⇓
Then blood reach to liver and in hepatocyte
unconjugated bilirubin convert into conjugated bilirubin by glucuronosyl
transferase
⇓
Then conjugated bilirubin by biliary system goes to small intestine
⇓
In Small intestine conjugated bilirubin à urobilinogen
⇓
Here urobilinogen 90% excreted by faeces so sometimes
yellow faeces seen.
⇓
While 10% urobilinogen by portal vein to blood and
excreted by kidney so abnormal intense yellow urine seen.
Toxic or intrahepatic jaundice
- Both unconjugated and conjugated bilirubin accumulate in the blood
- Damage
to liver cells may impair both conjugating and secretory
mechanisms
Etiology
- Bacteria : Salmonellosis and Leptospirosis
- Virus : Infectious canine hepatitis(ICH)
- Phytotoxins : crotalaria and Senecio
- Chemicals : Phosphorus, chronic copper poisoning, chloroform, carbon tetrachloride.
- Acute or chronic hepatitis, hepatotoxicity, cirrhosis, Necrosis
Cell necrosis reduces the liver's ability to
metabolize and excrete bilirubin and unconjugated bilirubin in the blood
⇓
The blood contains an abnormally raised amount of
conjugated bilirubin and bile salts which are excreted in the urine
NOTE
: Both unconjugated and conjugated bilirubin accumulate in the blood
⇓
Acute or chronic hepatitis or biliary cirrhosis
leading to an increase in plasma conjugated bilirubin because there is
excretion of conjugated bilirubin into the bile
⇓
Here unconjugated bilirubin still enters the liver
cells and becomes conjugated
⇓
So this conjugated bilirubin is returned into the
blood by rupture of the congested bile canaliculi and direct emptying of the
bile into the lymph leaving the liver
⇓
So most of the bilirubin in the plasma becomes the
conjugated than the unconjugated type
⇓
And this conjugated bilirubin which not goes into
intestine to become urobilinogen gives the
urine the dark color.
Obstructive or post hepatic jaundice
- secretion (excretion) of conjugated bilirubin is impaired
- Grey or putty like faeces
- Urine contain bilirubin
Etiology
- Blocking of bileduct from within
Ascaris
lumbricoides in swine
Thysanosoma
astiniodes (fringed tape worm)
Fasciola
gigantica in cattle
Gall
stones
- Pressure on bile duts from outside by Fibrosis, Abscesses, Enlarged pancreas or lymph nodes
Granulomas, Tumours,
- Inflammatory processes in biliary system like
Dicrocoelium
dendriticum
cholecystitis
fascioliasis,
- Closure of bile duct due to Duodenitis and thickening of mucosa
- Biliary atresia,
- Cholangiocarcinoma,
- Pancreatitis are also responsible.
Pathogenesis
In complete obstruction
of the bile duct
⇓
Not found urobilinogen
in the urine, so bilirubin has not access to the intestine
⇓
and in the intestine the
bilirubin converted to urobilinogen to be later released into the general
circulation of animal body
⇓
Presence of bilirubin (conjugated) in the urine without urine-urobilinogen suggests obstructive jaundice
⇓
Also if presence of pale
stools and dark urine suggests an obstructive or post hepatic.
Clinical sign
Prehepatic Jaundice Hepatic
Jaundice
Intravascular or extravascular anaemia Weight
loss
Weakness Anorexia
Pale mucous membranes
Ascites
Tachycardia and tachypnea Vomiting
and Diarrhoea
Haemoglobinemia Polydipsia/polyuria
Haemoglobinuria ('port wine' urine) Coagulopathy
and
Hepatoencephalopathy
Post
hepatic Jaundice
- If complete obstruction so pale gray faeces
- Bleeding disorders
- If acute pancreatitis so seen anorexia, vomiting, diarrhoea and abdominal pain in animals
- If jaundice is associated with biliary rupture so resorption of bile pigments and accumulating in the peritoneal cavity and ascites.
Diagnosis
Base on the…
- Hematology Parameter
- Serum biochemistry
- Urinalysis
- Faeces
If presence of Jaundice in tissue
⇓
Perform Complete Blood Count(CBC) and
Serum Biochemistry
⇓
If hyperbilirubinemia is conformed so
seen the PCV/HCT
⇓
If PCV/HCT < 15% so it is pre hepatic
Jaundice
⇓
But If PCV/HCT >= 15% so next step is ultrasonography (USG)
⇓
In USG If bile duct and Gall bladder not dilated
so hepatic Jaundice
⇓
If bile duct and Gall bladder dilated so it is Post hepatic Jaundice.
Van den Bergh Reaction
It is used for determine type of bilirubin
- mixing
Ehrlich's reagent (diazotized sulphanilic acid) with plasma or serum
- form
a colored compound known as azobilirubin
Direct
: Immediate reaction
with conjugated bilirubin : pink or purple
obstructive jaundice
Indirect: Unconjugated bilirubin gives a delayed reaction:
Within 10 minutes, a golden colour appears - haemolytic jaundice
Biphasic
reaction: a brownish-red colour appears during the
first two minutes, - toxic jaundice
Differential Diagnosis of
jaundice
Parameter Haemolytic Toxic Obstructive
Bilirubin Increase unconjugated Increase conjugated & Increase conjugated
Increase unconjugated
Van de bergh Indirect
Biphasic
direct
Urine bilirubin -
+ +
Urnine Slight present not
Urobilinogen present present
Liver Function Negative Positive Negative
Test
Serum Normal Decrease Increase
Colostrum
Haemoglobinuria Present Absent Absent
Faeces Intense yellow Normal Pale or
Greyish
No smell foul
smelling
Macroscopic Pathology
- First identify the primary cause of jaundice.
- Haemolytic jaundice : prevent the haemolysis and Given Haemoprotozoan drugs.
- Obstructive jaundice : Find the cause of obstruction If there are endoparasite so given anthelmintic drug. If there is any neoplasm growth or stone so surgically removal.
- Toxic jaundice : Treatment as a hepatitis.
- Fluid therapy : Dextrose (DNS) Orally or Panretally.
- Suggest for Fat free and salt free diet.
References
https://www.vin.com/doc/?id=7259263
https://en.wikipedia.org/wiki/Jaundice
ecoursesonline.iasri.res.in/mod/page/view.php?id=130402
labpeda.net
(A Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
(ACourtesy School of Veterinary Medicine, Purdue University.)
(ACourtes Dr. A. Confer, Center for Veterinary Health sciences, Oklahoma
State University.









Great work Dr.... Very nice information 👌👌👌👍
ReplyDeleteNice information about jaundice
ReplyDeleteHello, this was very helpful. I just came across this incredible gastro doctor in Ludhiana at Girn Hospital. Their medical services are very reliable and efficient.
ReplyDeletePost a Comment