What is colic?
The term “colic” is defined as a general manifestation of abdominal discomfort in the horse, regardless of the cause.
While most cases of colic are associated with gastrointestinal disturbances, the nature of some abdominal discomfort may be non-gastrointestinal in origin, such as those resulting from other abdominal organs (including but not limited to the liver, spleen, ovaries, or kidneys).
Colic is classified as abdominal pain or pain within the digestive tract due to a gastrointestinal disturbance.
Colic is not a disease but a group of symptoms.
Classification / types of equine Colic
Anatomical: -
1.
True colic and
2. False colic
Etiological colic: -
1.
Physical colic and
2.
Functional colic
Clinical colic: -
1. Spasmodic colic
2. Tympanic colic
3. Obstructive colic
4. Extra-luminal colic
Based on duration of the disease
1. Acute: <24-36hrs
2. Chronic: >36hrs
3. Recurrent: multiple episodes separated by periods of >2days of normality.
% of Various Type of colic reported on a farm based survey
Non-specific diagnoses 64% 1
Impactive/acute intestinal obstructive colic 17%
Spasmodic colic 9%
Sand colic 5%
Gas colic 3%
Verminous mesenteric arteritis 1%
Enteritis due to ingestion of moldy grain 1%
Risk Factor
Identified a number of factors that are associated with increased risk of colic are
The intrinsic factors of horses (age, breed & sex)
Parasite Burden
Certain feed types
Recent change in feeding practices
Stabling
Lack of access to pasture and water
Increasing exercise and transport
Daily feeding of concentrate > 5 kg/day to horses increased the risk of colic.
Feeding more than twice daily increased the risk of colic.
Feeding ≥ 50% of the diet as alfalfa, feeding <50% of the diet as oat hay and lack of daily access to pasture grazing are found to be significantly associated with Colic.
Activity:
Decreased in regular exercise or changing from turn out activity to strict stall confinement increased risk of cecal and large colon impaction.
Transport >24 hours increased risk of simple colonic obstruction or distension.
Cribbing behaviour may increase the risk of simple colonic obstruction or distension.
Parasites:
Parascaris equorum causes the Small intestinal obsruction without infarction.
Anoplocephala perfoliata increased risk of bowel irritation, ileal impaction and spasmodic colic.
Large strongyle worms, most commonly Strongylus vulgaris, are implicated in colic secondary to non-strangulating infarction of the cranial mesenteric artery supplying the intestines.
Pathophysiology
Simple
obstruction
Trapping
of fluid within the intestine
The
large amount of fluid produced in the upper gastro-intestinal tract
This is
primarily re-absorbed in parts of the intestine downstream from the
obstruction.
This
degree of fluid loss from circulation leads decreased plasma volume leading to
a reduced cardiac output and acid-base disturbances.
Intestine
distention due to the trapped fluid and by gas production from bacteria
Activation
of stretch pain receptors leads to the pain
With
progressive distension there is occlusion of blood vessels, firstly veins then
arteries.
Impairment
of blood supply
Leads
to hyperemia and congestion and ultimately to ischemic necrosis and cellular
death.
Leading to an increased permeability.
In the
opposite fashion gram-negative bacteria and endotoxins can enter into the
bloodstream leading to further systemic effects
Obstructive
+ Strangulating
⇓
Distention loss of barrier function
⇓
Impairment of blood Supply
Critical reduction in
blood flow and tissue perfusion leads to tissue hypoxia/ ischemia
Epithelial cells
begin to loosen at villus tip lead to Necrosis
Cardiovascular
collapse & Endotoxemia
Inflammation
Increase GI motility
and decrease absorptive function (causing diarrhoea)
Accumulation of fluid
and ingesta
Distention
Abdominal pain due to
stretching of the wall
Symptoms of Colic
Loss of appetite
Increased pulse rate
Excess salivation
Frequent attempts to urinate or defecate
Abdominal pain
Pawing
Stretching
Flank watching
Biting the stomach
Decreased faecal
output
Repeated lying down
and rising
Rolling
Categorization of abdominal pain
On the basis of the duration of action
Per
acute: <
1 hr
Acute:
<
24 hrs
Subacute:
24-72
hrs
Chronic:
>
72 hrs
On the basis of Character
Recurrent
Occasional
Intermittent
Continues
On the basis of the intensity
Mild
Moderate
Severe
Diagnosis
History and Clinical findings
Physical examination
Auscultation and percussion
Rectal examination
Nasogastric
intubation
Laboratory tests
Radiography
Ultrasonography
The described approach to colic workup is based on the
“10 P’s” of Dr. Al Merritt. You can use whatever approach you want. But, find
what works best for you then stick with it.
1. PAIN – degree, duration, and
type
2. PULSE – rate and character
3. PERFUSION – mucous membranes,
skin tent, jugular fill, etc.
4. PERISTALSIS – gut sounds, fecal
production
5. PINGS – simultaneous
auscultation/percussion
6. PASSING A TUBE – amount and character
of reflux, ifpresent
7. PALPATION – rectal exam
8. PAUNCH – a word for obvious
abdominal distention thatbegins with “P”
9. PCV/TP
10. PERITONEAL FLUID
History & clinical findings
History & clinical findings it gives clue for treatment, causes and whether the horse requires surgery.
Feeding practices, exercise, deworming, past episodes of colic and treatment given.
Respiration rate is
<
40/
min. in mild colic.
Up to 80 / min. in sever
colic.
>
120/min.
in terminal stage of colic.
Auscultation
Continuous and loud bolborygmi - Intestinal
hypermotility (Spasmodic colic, early
Absence or brief with Splashing
Character - ileus
Pinging sound - Small or large colon impaction,
gas colic or colon displacement, torsion of colon or cecum
The
heart rate gives a very good indication of severity of the colic and it also
gives a good idea of prognosis.
The more serious colic having very elevated heart rates.
Nasogastric intubation.
Passing a
Naso-Gastric Tube (NGT) is useful both diagnostically and therapeutically.
Diagnosis (
e.g.. Proximal bowel obstruction, gastro-duodenal ulcer, large colon
displacement)
Analgesia
Prevention of
gastric rupture
Administration of medication
In
general, gastric reflex up to 2 lit.
If excess Gastric out flow problem
Colour:-
Green or Brown Normal
Yellow S.I. reflex
Orange Haemorragic intestinal disease.
pH:-
4-6
Normal
6-8 Reflex from S.I.
Foul-smelling, fermented or copious bloody reflux is associated with anterior enteritis.
With intestinal obstruction, the reflux is usually composed of fresh feed material and intestinal secretions.
Reflux originating from the small intestine is alkaline whereas reflux composed of gastric secretions is acidic.
Rectal palpation
The rectal palpation helps to diagnose the type of colic which can be used to determine the treatment.
Rectal palpation helps to diagnose uterine torsion, viscus distension ( by gas, fluid or feces), large bowel displacement and dilated small intestinal loops.
The most important questions to answer when performing a rectal examination are:
Is visceral distention
present?
If so, which segment (i.e. large colon, small colon, cecum, or small
intestine) is distended?
What is the nature (i.e. fluid,
feed, gas, solid object) and severity (mild, moderate, severe) of the
distention?
Answers to these basic questions will provide diagnostic and/or therapeutic information for the majority of horses with colic, even if a specific lesion is not identified.
Abdominocentesis
The extraction of fluid from the peritoneum can be useful in assessing the state of the intestines.
Radiography:
Abdominal radiographs used to diagnose the colic due to
Enteroliths and Sand impaction.
The abdomen radiography is divided into 3 regions using
the following techniques:
Cranial (140 kvp, 120 mAs, 500 mA)
Mid abdomen (140 kvp, 160 mAs, 500 mA)
Caudal aspect (140 kvp, 100 mAs, 500 mA).
Laboratory tests
Increase PCV and TP Indicate
dehydration.
Complete blood count
Proximal Entritis –
leucocytosis with left shift,
Peritonitis – leucocytosis
& increase fibrinogen concentration.
Endotoxaemia – marked
leucopenia
Serum electrolyte profile
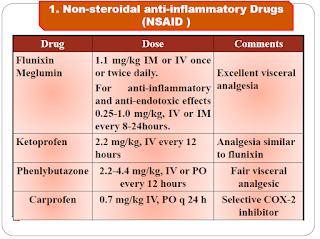
Medical management of colic
Most causes of colic can be managed medically only a 4% to 10% require
surgery.
The decision whether a colic case should be managed medically
or surgically depends on 5 main points.
Severity of pain (responsive vs. Nonresponsive to analgesia),
Cardiovascular and systemic status
Findings on transrectal palpation
The presence of nasogastric reflux
Results of abdominocentesis
Treatment outline:
Correction of pain
Hydration therapy
Replacement therapy,
Maintenance therapy
Other therapy
Antibiotics
Lubricants
Fecal softeners
Promotility agents
Antiulcerative therapy
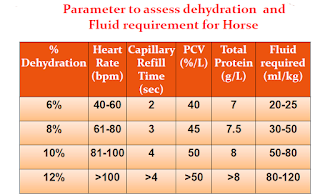
Fluid therapy plan
Correction of dehydration:
Estimate of dehydration (%) x body
weight (kg)
Volume of fluids to give:
Maintenance requirements + Correction of
dehydration + Ongoing losses
For example,
A 500 kg horse that is 6% dehydrated would require approximately 30 liters to correct the fluid deficit.
Maintenance fluid requirements for the adult horse are approximately 50-60
ml/kg/day or approximately 25-30 liters per day.
As an example, assume you are presented with
a 500 kg horse afflicted with colitis. The horse has had diarrhea for 2 days,
is off feed, and clinical examination findings result in an estimate of
moderate (7%) dehydration.
A plan for the initial 12 hours would be formulated as
follows:
1. Rehydration needs: 0.07 (estimated 7% dehydration) x 500 kg = 35 kg ≈
35 lit.
2. Maintenance needs: 50 mL/kg/24 h x 500 kg = (25,000 mL/24 hours)/2 =
12.5 lit.
3. Ongoing losses: estimated at 2 lit./h x 12 h = 24 lit.
TOTAL:
35 + 12.5 + 24 = 71.5 lit.
1. Dehydration
fluid deficit in liters:
Equal to the weight of the horse in kilograms times the
percent dehydration.
2. Daily
maintenance needs of the horse in liters:
60 ml/kg/day (adult)
70-80 ml/kg/day (foal)
3. Fluids needed
for ongoing losses:
Such as fluids lost in diarrhea or nasogastric reflux.
Combination of clinical signs and basic laboratory
tests can be used to assess hydration.
69
The composition of the fluids to be administered
should be selected based upon the most likely fluid and electrolyte needs and
upon results of a chemistry profile.
Frequently, a balanced polyionic fluid, such as
lactated or acetated Ringers, is appropriate. However, sometimes it is
necessary to administer other types of fluids.
The most common electrolyte abnormalities that develop
are hypokalemia and hypocalcemia; these are often exacerbated by administration
of high volumes of IV fluids, particularly in horses that are not allowed to
eat.
Horses with gastric reflux often develop hypochloremic
metabolic alkalosis; these horses should probably be administered 0.9% NaCl
with KCl.
The most common acid-base disturbance encountered is metabolic acidosis,
which occurs as a consequence of lactic acidosis secondary to hypovolaemia
and/or endotoxaemia, or of hyponatraemia secondary to colitis, peritonitis or
gastrointestinal torsion.
Metabolic alkalosis occurs as a consequence of hypochloraemia secondary
to high volume gastric reflux or of hypoalbuminaemia.
Treatment should be aimed at the underlying cause, thus, lactic acidosis
should be treated with a large volume of polyionic fluids, hyponatraemia with
normal or hypertonic saline, hypochloraemia with normal saline and
hypoalbuminaemia with colloids.
Prevention:
Maintain a regular feeding schedule.
Ensure constant access to clean water.
Provide at least 60% of digestible energy from forage.
Do not feed moldy hay or grain.
Feed hay and water before grain.
Provide access to forage for as much of the day as possible.
Do not over graze pastures.
Do not feed or water horses before they have cooled out.
Maintain a consistent exercise regime.
Control intestinal parasites through periodical deworming programme.
Sources:
https://lacs.vetmed.ufl.edu/files/2011/12/Equine-Colic-and-GI-Diseases.pdf
https://secure.caes.uga.edu/extension/publications/files/pdf/B%201449_1.PDF
https://pubmed.ncbi.nlm.nih.gov/15631904/
https://www.researchgate.net/publication/242192389_Colic_prevalence_risk_factors_and_prevention
https://nurseslabs.com/nasogastric-intubation/
https://www.slideshare.net/hamedattia1/colic-in-equines-prof-dr-hamed-attia-74345874




















Post a Comment